Reviewing Breathing Sensors as a Tool for Workload Monitoring
This article explores if breathing sensors and respiratory metrics improve training workload monitoring compared to heart rate. We examine their link to RPE and scientific insights on its deployment.
When coaches and athletes talk about tracking training, they often look at it from multiple angles to help them truly understand the load and recovery process [1, 2]. Generally, this breaks down into three main areas: the work done, the body's response to that work, and how the athlete feels about it.
The 'work done' is what's called external workload – the objective metrics like how fast, how far, how long or the power produced on a bike. It's simply measuring the physical task itself.
Then there's the internal workload. This is about how the body is handling that external work. It's the physiological reaction; things like heart rate or lactate levels.
Finally, there's the subjective feeling. This is the athlete's perception – how hard it felt and how fatigued they are, often captured through things like a rating of perceived exertion (RPE) or post-activity comments. It's a crucial piece that objective numbers might miss.
For a long time, especially when training out in the field, tracking internal workload has mostly meant keeping an eye on heart rate. Heart rate monitors became popular because they're easy to use, affordable and relatively cheap.
But what if heart rate doesn't tell the whole story? What if there's another physiological signal that could offer a different, maybe even more direct, window into the body's effort level during activity? Recent developments are pointing towards using breathing as a metric for internal workload and new wearable tech has be popping up as a reaction to this research. The buzz around this new development has reached such levels that even the UCI is planning to ban its use. However, this also raises interesting questions: How exactly does tracking breathing work in practice? Can it really provide valuable insights for athletes? And what does the actual science say about its potential?
The Gold-Standard Ain’t So Shiny After All
Heart rate has become the most widely adopted metric for tracking internal workload in the field, easily accessible on most wearables and often considered a key indicator of effort and fitness.
However, understanding what heart rate data truly represents can be complex. As highlighted in research, such as a notable review by Jeukendrup and Van Diemen, heart rate is significantly influenced by numerous factors beyond the athlete's work output. These confounding variables can make precise interpretation challenging even for experienced coaches.
The research discuss several scenarios where heart rate can be misleading. A prominent example for endurance athletes is cardiac drift, where heart rate gradually rises during prolonged exercise even when the external workload remains constant. They note that heart rate can increase by up to 20 bpm during efforts lasting 20-60 minutes. This phenomenon means that to maintain a stable heart rate later in a workout, an athlete might have to progressively reduce their workload, with some situations necessitating reductions up to 17%.
The review further points out that heart rate is sensitive to other environmental and physiological conditions unrelated to current effort. These include factors like altitude, hydration, lack of sleep, air and core body temperature, and even body position (such as on a bike). While not specifically detailed in that review, it's also widely known that stimulants like caffeine or psychological factors such as stress or excitement can influence heart rate.
Because of this multitude of influencing factors, relying solely on heart rate to accurately quantify training workload or measure subtle performance progress becomes difficult. While combining it with subjective metrics like RPE is an improvement, there is a clear benefit in exploring other objective and portable measures to get a better understanding of internal workload.
This is where new technologies focusing on different physiological signals are beginning to show potential.

The New Kid On The Block: Breathing Rate
Building on the need for more reliable internal workload metrics beyond heart rate, another physiological signal is gaining attention in wearable technology: breathing.
The premise gaining traction, and discussed widely by Dr. Seiler in a podcast, suggests that respiration rate could align closely with how hard an athlete feels they are working (perceived exertion). This potential alignment is sometimes attributed to common neurological control centers governing both breathing and subjective feelings of effort.
Furthermore, a key claimed advantage is that, unlike heart rate, breathing metrics are said to be less susceptible to confounding factors such as stress, stimulants hydration, environmental temperature or altitude. This potential stability could offer a more consistent measure of internal load. It's also proposed that breathing responds more immediately to changes in effort, potentially providing a quicker and more accurate reflection of stress during intermittent, high-intensity activities compared to heart rate, which can exhibit a noticeable lag.
However, even proponents acknowledge that breathing metrics are not entirely immune to variability. Like cardiac drift, respiration patterns can also exhibit a form of "drift" over prolonged exercise, suggesting that the internal breathing response isn't always a perfectly static mirror of constant external effort.
With companies like Tymewear beginning to commercialise wearable products designed to track these breathing metrics, and with Dr. Seiler himself involved in their design and marketing process, it becomes crucial for those interested in evidence-based research to ask what the existing peer-reviewed science actually say about these claims.
This article aims to explore the available scientific literature to understand whether this technology is grounded in science or whether we are being sold snake oil.

From Marketing to Science
With the concept of breathing metrics emerging, it's helpful to look at specific products entering the market. Tymewear is one company offering a breathing sensor, the VitalPro strap, which combines both heart rate and respiration rate monitoring in a single chest unit. However, their product comes with a hefty price of $299, which is roughly three times more than other heart rate monitors which also track breathing rate.
Examining their marketing, Tymewear focuses on the capability of their technology to predict key physiological indicators such as ventilatory thresholds and intensity zones. The promise here is that by using breathing data, athletes can gain precise insights to target specific intensity levels during their training sessions.
Given these claims and the current buzz surrounding this type of technology, it is valuable to critically examine the scientific basis behind these claims. The remainder of this article will delve into existing peer-reviewed research to explore whether the science supports the potential of breathing metrics to deliver on these promises.
Specifically, we will seek to answer the following questions which are directly related to the core functionalities claimed:
Is it possible to accurately measure respiratory frequency through a chest strap?
How strong is the relationship between respiration rate and an athlete's rate of perceived exertion (RPE)?
Can physiological thresholds, such as ventilatory thresholds, be reliably derived from respiration rate?
To what extent might environmental or physiological factors confound or affect the accuracy and interpretation of respiration rate data?
Accuracy of Wearable Respiratory Sensors
While laboratory methods for measuring respiration rate often involve precise equipment like face masks or flow sensors that directly quantify air movement, these are impractical for use during dynamic exercise in the field. This is why wearable devices, particularly chest straps, are explored as an alternative, inferring respiratory patterns from the movement of the chest. The key question for athletes and coaches is: how accurately can these practical, commercially available devices measure respiration rate?
A research team led by Nicolò in Rome investigated this very question by comparing the accuracy of several commercially available wearable devices against a flow sensor. Their study tested various devices, which use various sensor technologies, during different exercise intensities. They found that while the wearable devices showed a relatively small average difference (around 0.5 breaths per minute) compared to the reference sensor, there was notable variability in the results depending on the specific device and conditions. The authors suggested that ongoing refinements in the algorithms and hardware of these devices could lead to improved accuracy. In fact, additional research is regularly being released proposing newer technologies in an attempt to get more accurate respiratory frequency results.
Another Italian research group published a study in 2015 focusing on elite male football (soccer) players. They compared respiration rate data from a chest strap against measurements from a face mask during an incremental test performed on a treadmill. They reported an overall error rate of 5.24% for the chest strap compared to the mask. The researchers concluded that this level of accuracy was likely sufficient for many in-field applications in sports. However, they also noted that their testing was done on a treadmill, and the accuracy might be different during actual football play involving dynamic movements, jumps, or physical contact.
Earlier validation efforts also contributed to understanding the potential of such technology. For instance, research by J.-H. Kim et al. and Hallstone et al., published in 2013 and 2011 respectively, compared the respiration rate measurements from the Zephyr BioHarness to clinical-grade devices. These studies generally found good agreement, concluding that the BioHarness could provide valid and reliable respiration rate data comparable to medical equipment, particularly during moderate to high-intensity exercise, suggesting that the accuracy can depend on the intensity of the activity.
Connecting Respiration Rate to RPE
Now that we've seen that accurately measuring respiration rate with wearable chest straps is a feasible approach, the next crucial question is whether there is a relationship between this physiological measurement and the athlete's perception of effort. One key way coaches and athletes gauge training intensity is through Rate of Perceived Exertion (RPE) – a subjective scale reflecting how hard an activity feels, which will serve as our comparable metric.
A study by Leonardo de Almeida e Bueno et al. published in 2018 investigated the relationship between RPE and various physiological parameters in recreational runners. Using precise laboratory equipment during exercise tests, they measured multiple cardio-respiratory factors. When comparing these objective measures to the athletes' reported RPE, they found that minute ventilation (breathing volume per minute) showed the strongest correlation with RPE, even more so than heart rate. While this specific finding regarding minute ventilation's correlation was drawn from a small subset of 5 participants, it highlights a potential strong link between overall respiratory dynamics and perceived effort.
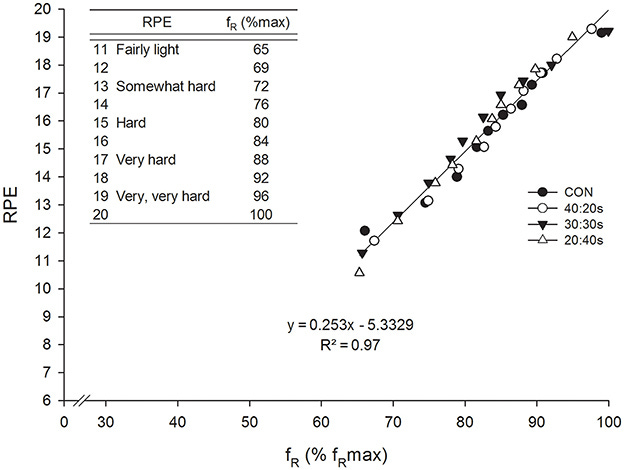
Further studies by Nicolò et al. provide additional insights, focusing specifically on respiratory frequency. In a 2015 study involving trained cyclists, a strong relationship between respiratory frequency and RPE across various exercise tests up to 30 minutes in duration was found. This relationship was more pronounced than the relationship derived by other collected metrics such as heart rate, leading the authors to suggest that respiratory frequency is the most closely related metric to RPE within the durations investigated.
A subsequent study performed in 2019 once again by Nicolò et al. noted a significant correlation between RPE and both respiratory frequency and heart rate in football (soccer) players. Notably, they also observed that respiratory frequency seemed to respond more quickly than heart rate during the rapid work and recovery cycles typical of intermittent sports, suggesting it might be a more timely indicator of fluctuating effort.
Deriving Ventilatory Thresholds from Respiratory Data
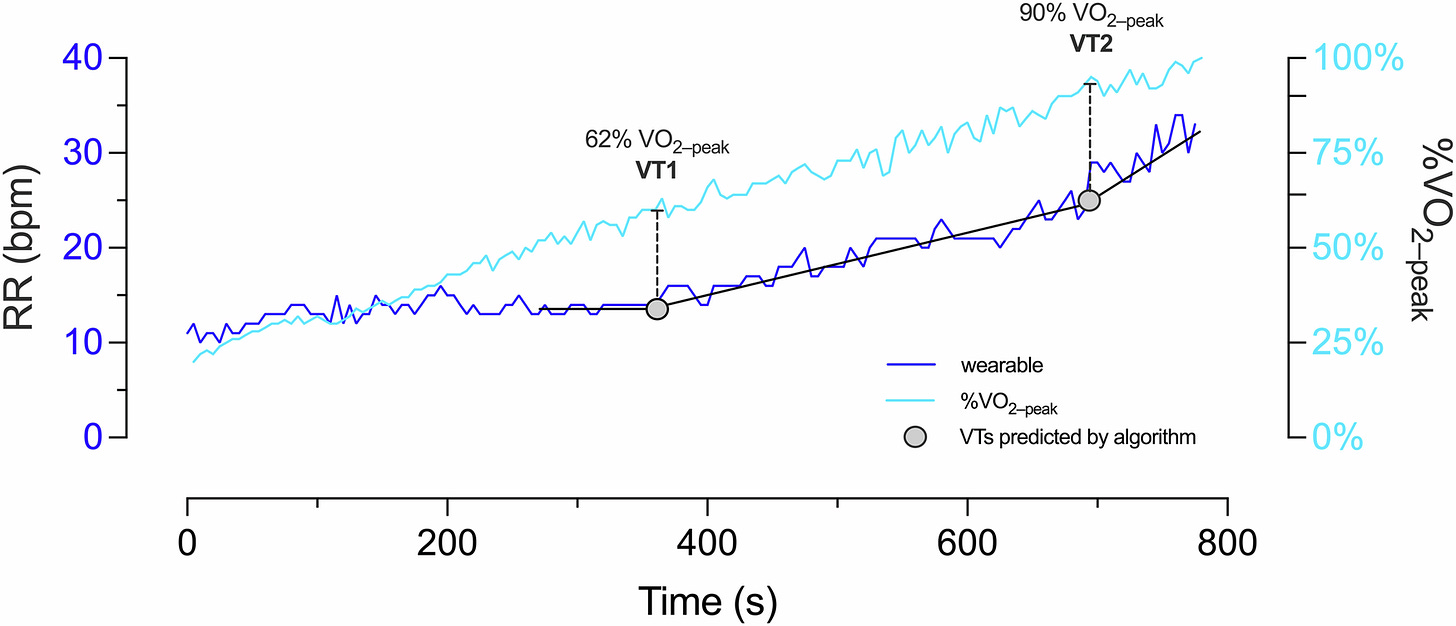
Beyond simply reflecting how hard an effort feels, we need to understand if respiration rate also help pinpoint specific physiological intensity markers. Athletes and coaches frequently use thresholds like ventilatory thresholds (VT) for this purpose. Ventilatory thresholds, typically identified as VT1 and VT2, represent points during increasing exercise intensity where breathing patterns change noticeably. VT1 marks the transition from primarily aerobic exercise to increased reliance on anaerobic metabolism, while VT2 signifies the point where breathing becomes significantly laboured as the body struggles with the increased intensity. Being able to accurately derive these thresholds from respiratory data would be very useful for training prescription, directly relating to claims about predicting zones.
In 2021, a Spanish research group investigated whether ventilatory thresholds derived from respiration rate data correlated with thresholds determined by standard physiological methods and heart rate data in sportsmen during a cycling test. They found a strong agreement, showing that the ventilatory thresholds estimated from respiration rate were closely aligned with those determined by standard, more complex methods, as well as thresholds derived from heart rate. Their results indicated that the estimation was consistently more accurate for the second ventilatory threshold (VT2) rather than for the first (VT1).
However, findings are not entirely uniform across studies. A more recent study published in 2024 also examined the accuracy of respiratory frequency-derived ventilatory thresholds during cycling ramp tests in trained athletes, comparing them against reference values from medical-grade equipment. Interestingly, their results showed a high correlation between the estimated and actual first ventilatory threshold (VT1), alongside a moderate correlation for the second ventilatory threshold (VT2). This presents a contrast to the previous study, suggesting that external factors like the methodology or device used might influence the results.
The relevance of estimating ventilatory thresholds is further underscored by studies linking them to other key physiological markers used in training. An adjacent area of research, such as the 2018 study by Elmer and Toney, has investigated the relationship between ventilatory thresholds and lactate thresholds (LT). Their work found a strong correlation between the second ventilatory threshold (VT2) and the second lactate threshold (LT2) however, they didn’t comment on the relationship between the first thresholds (VT1 and LT1). This research provides scientific context for why identifying VT from metrics like respiration rate is valuable – it offers a basis for determining training zones often defined by lactate levels, aligning with the functional claims made by breathing sensor technologies.
Real-World Influences on Respiration Rate
We've reviewed evidence suggesting that respiration rate can be measured by wearable chest straps and that it correlates with subjective effort (RPE) and shows promise for deriving physiological thresholds (VT). But how reliable is this data when faced with the various factors encountered during real-world training such as environmental conditions and the athlete's own physiological state? As we noted earlier, heart rate is known to be influenced by many factors beyond exercise intensity and it’s important to understand if respiratory metrics are less susceptible to these confounding factors.
Currently, comprehensive research specifically testing the accuracy and validity of respiration rate measurements from wearable chest straps across a wide range of different environmental or physiological states is still relatively limited.
However, different tests employed by a previously referenced study by J.-H. Kim et al. on the Zephyr BioHarness were performed in environments with different air temperatures (22°C and 32°C). Their findings indicated that the device maintained comparable accuracy across these tested temperatures.
Furthermore, as mentioned in the section on RPE, research by Nicolò et al. (2019) on footballers noted that respiration rate shows a faster response to quick changes in exercise intensity and recovery compared to heart rate. This is another characteristic difference between the two metrics.
Beyond environmental factors, the type of activity itself can influence breathing patterns, which is important for interpreting respiration rate data. A study published in 2012 compared breathing patterns during treadmill running and cycling at similar relative exercise intensities in both trained and recreationally active individuals. They found that at the same relative effort level, respiratory frequency (breaths per minute) was higher during running, while tidal volume (the amount of air inhaled per breath) was lower compared to cycling. Notwithstanding the difference in modalities, the overall minute ventilation (total air breathed per minute, which is frequency multiplied by volume) was relatively similar. The authors theorised that these modality-specific differences relate to varying muscle activation patterns. This highlights that simply looking at respiratory frequency in isolation is not enough, and it might need to be interpreted with the context of the specific sport, as the body's overall breathing strategy can vary. Their study also observed that respiratory frequency at matched relative intensities was similar between the trained and recreationally-trained groups, suggesting that the athleticism of the individual is not a confounder of respiratory monitoring.

Your Next Key Metric Might Be Hiding in Plain Sight
To circle back to where we started, the motivation for diving into the science of respiratory metrics stemmed from the emerging buzz around new commercial products like the Tymewear strap and the discussions they've sparked. It's important to reiterate that the aim here was not to review or endorse any specific product, as that would require hands-on testing, but rather to investigate the scientific basis behind the types of claims being made.
What the journey through the research literature suggests is that the core ideas have scientific plausibility. Studies indicate that measuring respiration rate via wearable chest straps is indeed feasible with a reasonable level of accuracy for many contexts. Furthermore, there's evidence supporting a relationship between respiration rate and perceived exertion (RPE), and research shows promise for using respiration rate data to help estimate physiological intensity markers like ventilatory thresholds. While the science on how resilient respiration rate data is to environmental conditions or physiological states is still developing, initial findings suggest it might offer some positive improvements compared to heart rate.
Perhaps one of the most interesting practical takeaways from this exploration is the realisation that this technology might be more accessible than a brand new device might suggest. Many athletes already use heart rate chest straps that collect respiration rate data in the background. This data, often overlooked, is potentially already available in existing training logs, waiting to be explored.
For me personally, reviewing this research has certainly piqued my interest in utilising the respiration rate data that my current gear already collects. It appears there's a potentially valuable metric hiding in plain sight that could offer additional insights into training load and physiological response.
As this technology gains more attention, the collective experience of athletes experimenting with breathing rate data in real-world training becomes increasingly valuable. If you've already started looking at your breathing data, or if this article prompts you to start, please feel free to share your experiences, observations, and any challenges you've encountered in the comments below. Your insights can help build a broader understanding of how this metric functions in practice.


